Image commercially licensed from: Unsplash
Dr. Philippe Smith on Mental Health and Wellness: Insights from a Family Practitioner
In the tapestry of human health, mental wellness is an integral thread, often interwoven subtly yet significantly with our overall well-being. The importance of mental health profoundly impacts not only individual lives but also families and communities. In this context, the perspective of family practitioner Dr. Philippe Smith becomes invaluable. With his unique position at the frontlines of healthcare, Dr. Smith offers a holistic view of health that encompasses both the physical and mental aspects of the human experience. His insights connect the dots between mental health and physical wellness.
The landscape of mental health in family medicine is evolving rapidly. Gone are the days when mental health was a secondary consideration in general practice. Today, family practitioners are increasingly recognizing the importance of integrating mental health into routine care. They are often the first point of contact for individuals experiencing mental health challenges, placing them in a critical position to identify, manage, and, when necessary, refer patients to specialized care. This shift towards a more inclusive approach to health care is a reflection of the growing understanding that mental and physical health are deeply interconnected, and both are essential for a fulfilling, healthy life.
Understanding Mental Health in a Family Context
Family dynamics play a crucial role in shaping an individual’s mental health. These dynamics include the relationships and interactions between family members, communication patterns, and the overall emotional environment of the household.
“In a harmonious setting, where open communication, support, and understanding prevail, individuals tend to exhibit stronger mental resilience,” says Dr. Philippe Smith. “Conversely, in environments riddled with conflict, neglect, or abuse, the risk of developing mental health issues such as anxiety, depression, and stress-related disorders significantly increases.”
A family practitioner might encounter a case where a teenager presents symptoms of anxiety and depression. Upon delving deeper, it may become evident that the root of these symptoms lies in the family’s high-stress environment, characterized by parental conflict and unrealistic academic expectations. This scenario exemplifies how family dynamics directly impact an individual’s mental health.
Genetics also plays a pivotal role in mental health. Certain mental health conditions, like bipolar disorder, schizophrenia, and major depression, have a hereditary component, making individuals with a family history of these conditions more susceptibleIt’s essential to recognize that genetics is just one piece of the puzzle. The interaction between genetic predisposition and environmental factors often determines the likelihood of developing a mental health condition.
A family practitioner might observe a pattern where multiple family members across generations exhibit similar mental health challenges. Such observations underscore the need for a comprehensive family health history, enabling the practitioner to assess the genetic risks and provide targeted advice and interventions.
Common Mental Health Conditions in Family Practice
Throughout their careers, mental health practitioners and professionals encounter a range of mental health conditions in their clients and patients. The ability to recognize, diagnose, and manage these conditions is a vital component of providing comprehensive care. Among the most common conditions encountered are depression and anxiety disorders, each presenting unique challenges and requiring specific management strategies.
Depression is a prevalent mental health condition, often observed in family practice settings. It can manifest in various forms, ranging from mild to severe, and can significantly impact an individual’s daily functioning and quality of life. Symptoms of depression include persistent sadness, loss of interest in activities, changes in appetite or sleep patterns, fatigue, and feelings of worthlessness or guilt.
Notes Dr. Smith, “In diagnosing depression, family practitioners rely on a combination of patient self-reports, clinical observations, and standardized screening tools.”
Practitioners must differentiate between clinical depression and transient mood fluctuations. For example, a patient may present with symptoms of sadness and fatigue, but through careful evaluation, a practitioner might determine these symptoms are linked to a recent life stressor rather than clinical depression. This differentiation is essential for appropriate management.
Managing Depression in Family Practice
Initial management of depression in a family practice setting often involves a combination of therapeutic approaches. These may include counseling, lifestyle modifications, and, in some cases, pharmacotherapy. Family practitioners play a key role in educating patients about depression, addressing misconceptions, and collaborating with mental health professionals when necessary.
Importantly, the management of depression is not a one-size-fits-all approach. A patient with mild depression may benefit significantly from counseling and lifestyle changes, while another with severe depression may require a combination of medication and psychotherapy. Regular follow-ups are essential to monitor progress and adjust treatment plans as needed.
Anxiety Disorders: Recognition and Approach
Anxiety disorders, including generalized anxiety disorder, panic disorder, and social anxiety disorder, are also commonly encountered in family practice. These disorders are characterized by excessive worry, nervousness, or fear, which can be debilitating. Recognizing anxiety disorders can be challenging, as patients often present with physical symptoms such as palpitations, dizziness, or gastrointestinal disturbances.
“When diagnosing an anxiety disorder, family practitioners consider the duration and intensity of symptoms, as well as their impact on the patient’s daily life. They also rule out medical conditions that can mimic anxiety, such as hyperthyroidism or cardiac arrhythmias,” says Dr. Smith.
Initial Management of Anxiety Disorders
Initial management of anxiety disorders in a family practice setting involves patient education, counseling, and sometimes medication. Cognitive-behavioral therapy (CBT) is particularly effective for treating anxiety disorders and can be facilitated by trained practitioners or through referrals. In some cases, medications such as selective serotonin reuptake inhibitors (SSRIs) may be used to manage symptoms, particularly in moderate to severe cases.
Family practitioners also emphasize the importance of lifestyle modifications, such as regular exercise, adequate sleep, and stress management techniques, in the management of anxiety disorders. Early intervention and prevention are crucial in managing mental health conditions in family practice. Identifying and addressing symptoms early can prevent the progression of conditions like depression and anxiety disorders. Family practitioners are often in an ideal position to implement preventive strategies, such as screening for mental health conditions in patients with known risk factors or those undergoing significant life changes.
Preventive measures also include educating patients about the signs and symptoms of mental health conditions, reducing stigma, and encouraging open communication about mental health. For example, a family practitioner might provide resources or workshops on stress management and resilience-building, which are valuable for preventing anxiety and depression.
Integrative Approaches to Mental Health Care
In recent years, there has been a significant shift towards integrative approaches in mental health care, emphasizing the importance of treating the whole person rather than just the symptoms. This holistic perspective considers a variety of factors, including physical health, lifestyle, emotional well-being, and environmental influences, offering a more comprehensive approach to mental health care. Family practitioners, with their broad view of health and wellness, are ideally positioned to incorporate these integrative approaches into their practice.
Holistic mental health care involves a range of treatments that address the physical, emotional, social, and spiritual aspects of well-being. This can include traditional medical treatments like medication and psychotherapy, as well as complementary therapies such as acupuncture, yoga, or meditation. The goal is to provide a personalized treatment plan that caters to the individual needs of each patient. For example, a patient with anxiety might benefit from a combination of medication, cognitive-behavioral therapy (CBT), and mindfulness practices. This integrative approach not only addresses the immediate symptoms of anxiety but also equips the patient with long-term strategies to manage stress and improve overall well-being.
Collaboration with Mental Health Specialists
Collaborative mental health care involves a team approach, where family practitioners work alongside mental health specialists to provide comprehensive care. This collaboration can take many forms, from referrals to psychiatrists for complex medication management to working with psychologists for specialized psychotherapies.
In a collaborative care model, the family practitioner often acts as the coordinator of care, ensuring that all aspects of the patient’s health are addressed.
“A patient with severe depression might be referred to a psychiatrist for medication management while continuing to see their family practitioner for regular health check-ups and lifestyle advice. The family practitioner can also facilitate communication between different specialists, ensuring a cohesive and consistent approach to care,” says Dr. Smith.
Integrative and collaborative care models have numerous benefits, including improved patient outcomes, higher patient satisfaction, and more efficient use of healthcare resources. By treating the whole person and not just the illness, these approaches promote long-term well-being and empower patients to take an active role in their mental health care.
Navigating Mental Health Challenges During Life Transitions
Life transitions, whether predictable or unexpected, can significantly impact mental health. From the turbulent adolescent years to the complexities of parenthood and the challenges of aging, each phase of life brings its own set of mental health considerations. Family practitioners, who often see patients through various stages of life, play a crucial role in helping individuals navigate these transitions while maintaining mental wellness.
Adolescence: This developmental stage is marked by rapid physical, emotional, and social changes, often accompanied by heightened vulnerability to mental health issues like depression, anxiety, and eating disorders. Family practitioners are key in early detection and intervention, offering guidance and support to adolescents and their families.
Parenthood: The transition to parenthood, including pregnancy and the postpartum period, can be a time of significant emotional upheaval. Issues such as postpartum depression and anxiety are common, and family practitioners can provide essential support and resources to new parents navigating these challenges.
Aging: As individuals age, they often face a host of life changes, including retirement, health issues, and the loss of loved ones. These changes can lead to feelings of loneliness, depression, or anxiety. Family practitioners can help older adults manage these emotions and maintain a sense of purpose and connection.
Strategies for Resilience and Adaptability
Resilience, the ability to adapt well to adversity, trauma, or significant sources of stress, is crucial during life transitions. Family practitioners can guide patients in developing resilience through techniques like cognitive restructuring, stress reduction practices, and fostering strong social support networks. Adaptability is key to successfully navigating life transitions. Family practitioners can help patients develop this skill by encouraging a flexible mindset and teaching problem-solving strategies. They also can provide resources and referrals to support services as needed.
Family practitioners play an essential role in the early detection of mental health issues during life transitions. Regular check-ups and screenings can help identify problems early, allowing for timely intervention. Family practitioners often provide initial counseling and guidance to patients experiencing mental health challenges associated with life transitions. They can offer emotional support, practical advice, and referrals to mental health specialists when necessary.
In cases where long-term treatment is required, such as for chronic depression or anxiety disorders, family practitioners provide ongoing management and coordination of care. This might include medication management, regular monitoring of mental health status, and adjustments to treatment plans as needed. Family practitioners often connect patients with community resources, such as support groups, therapy options, and wellness programs. These referrals can be invaluable for patients seeking additional support during challenging life transitions.
Looking forward, the future of mental health in family medicine is promising and dynamic. It points towards a more integrated approach, where mental health is not seen as separate from physical health but as an essential component of overall well-being. This evolution in family medicine will likely involve greater collaboration with mental health specialists, increased use of technology in diagnosis and treatment, and a stronger focus on preventive care.
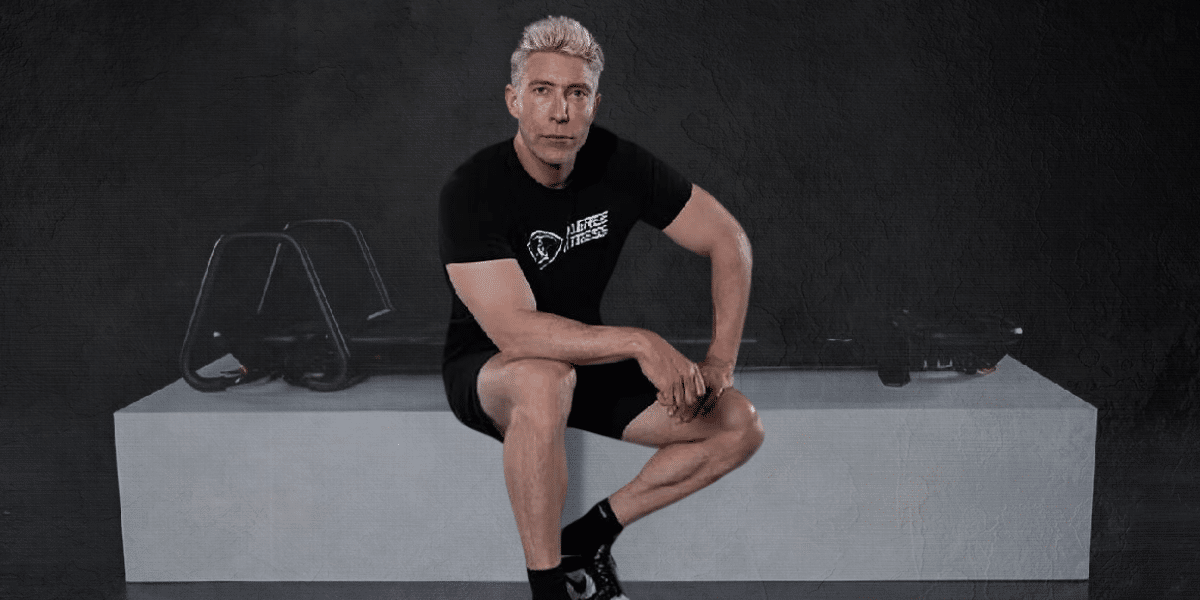
About Dr. Philippe Smith
Dr. Philippe Smith is a distinguished family practitioner who currently practices at Clinique Le Trait D’Union and Anna Laberge Hospital. Dr. Smith is dedicated to medical education has authored publications and actively contributes to charitable causes.